Bridging Specialties: Residents Lead Dermatology Didactics for Emergency Medicine

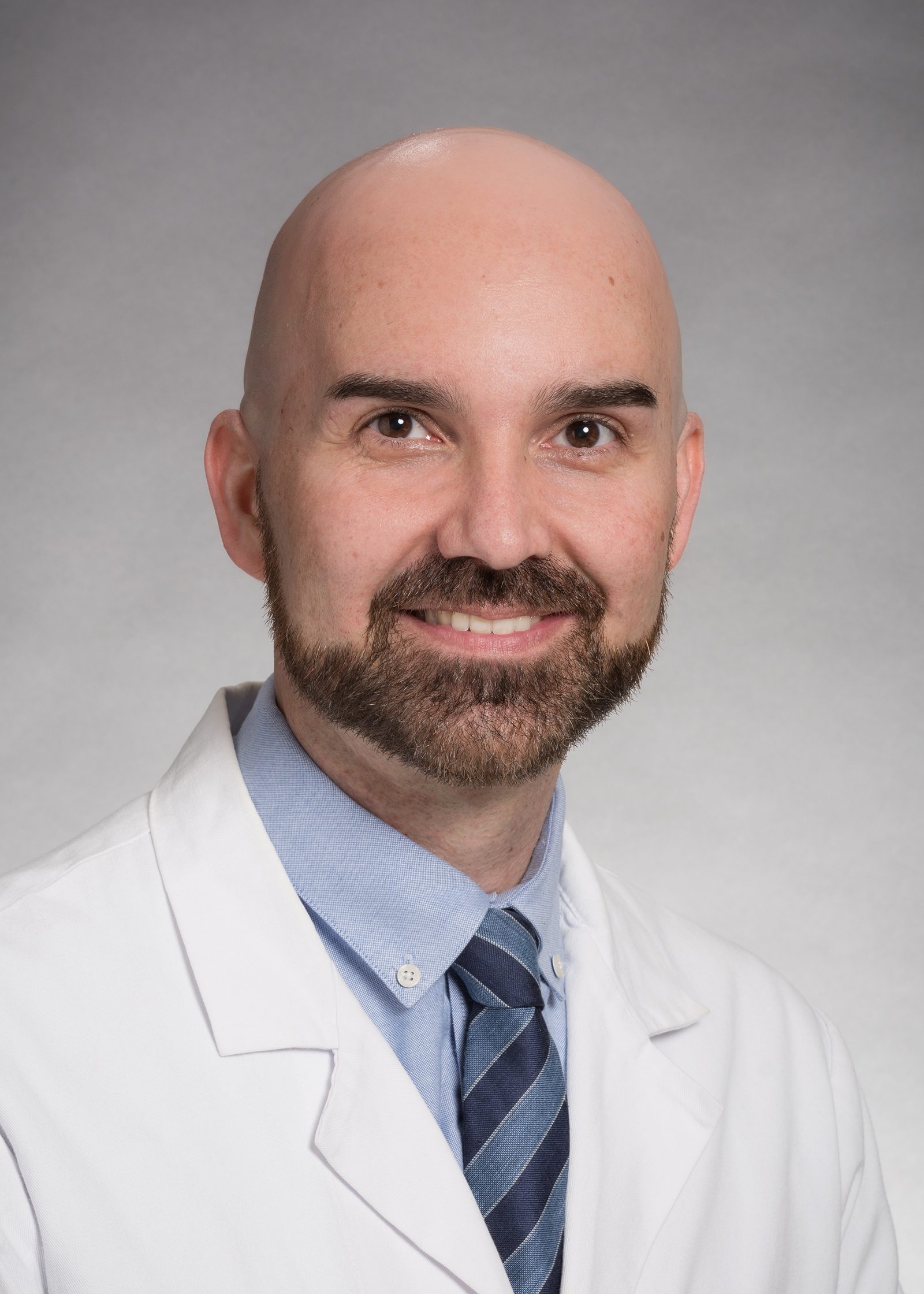
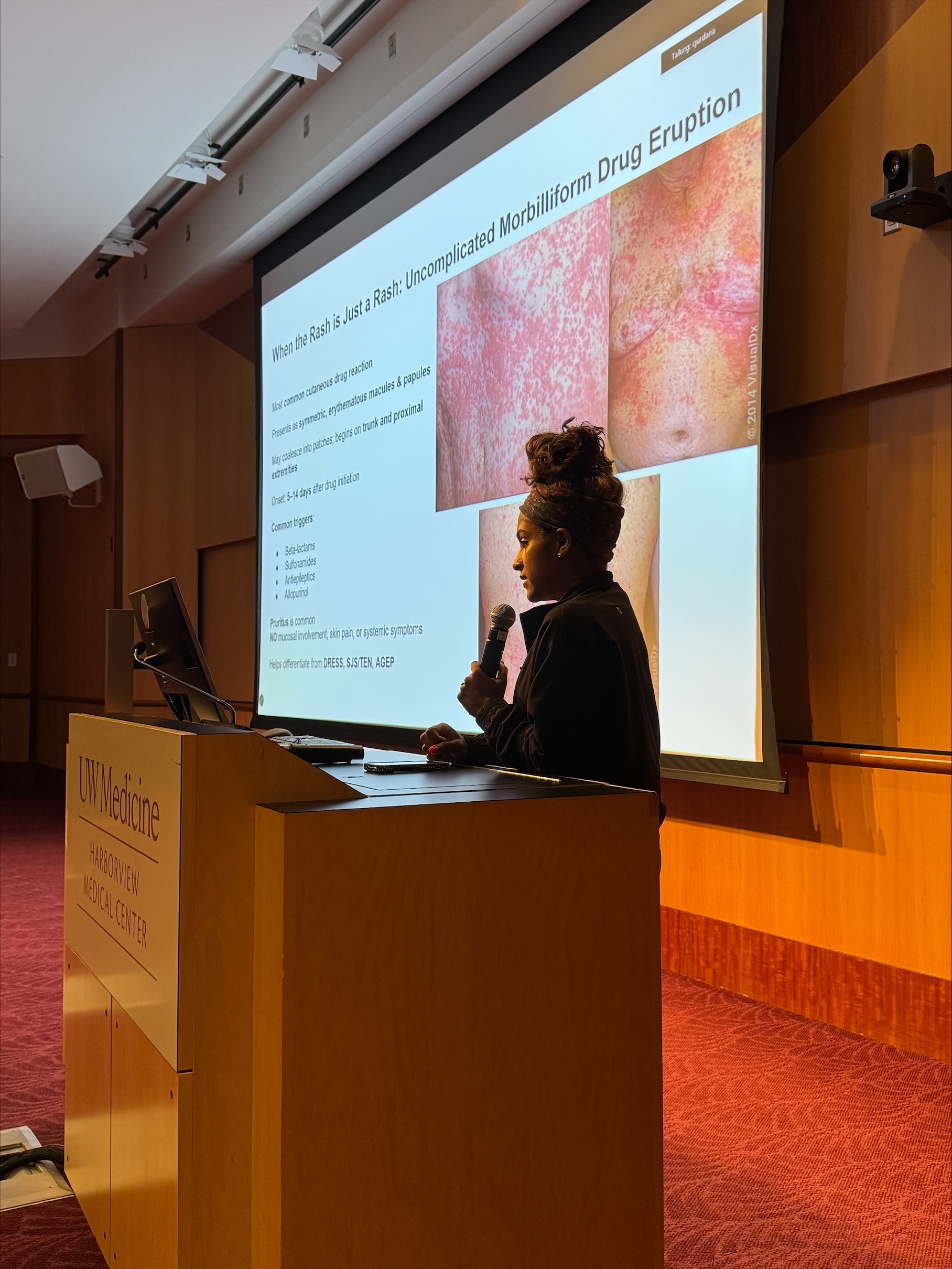
UW Dermatology's second-year residents—Drs. Marissa Appiah, Wenelia Baghoomian, and Pragna Naidoo—stepped into a teaching role this past Thursday, July 24, 2025, leading didactic sessions on dermatology for residents in the UW Department of Emergency Medicine.
Recognizing a gap in dermatology education among emergency physicians, the trio developed a tailored curriculum to help EM residents better recognize and manage both common and potentially life-threatening skin conditions.

In the Q&A below, Dr. Wenelia Baghoomian reflects on the importance of strengthening dermatology education in emergency medicine, and shares insights from her experience leading this resident-driven initiative.
Where did the idea for dermatology residents to teach emergency medicine residents originate?
The idea came from a shared recognition that dermatology is underrepresented in medical education, yet critically important, especially in the acute care setting. For many patients, their first interaction with the healthcare system for a skin condition is through the emergency department, not a dermatology clinic.
Since dermatologists aren’t always available in every hospital, we wanted to bridge that gap by empowering emergency medicine residents to feel confident identifying and managing common and life-threatening dermatologic conditions. Our goal was to demystify dermatology and give them practical tools to use on shift.

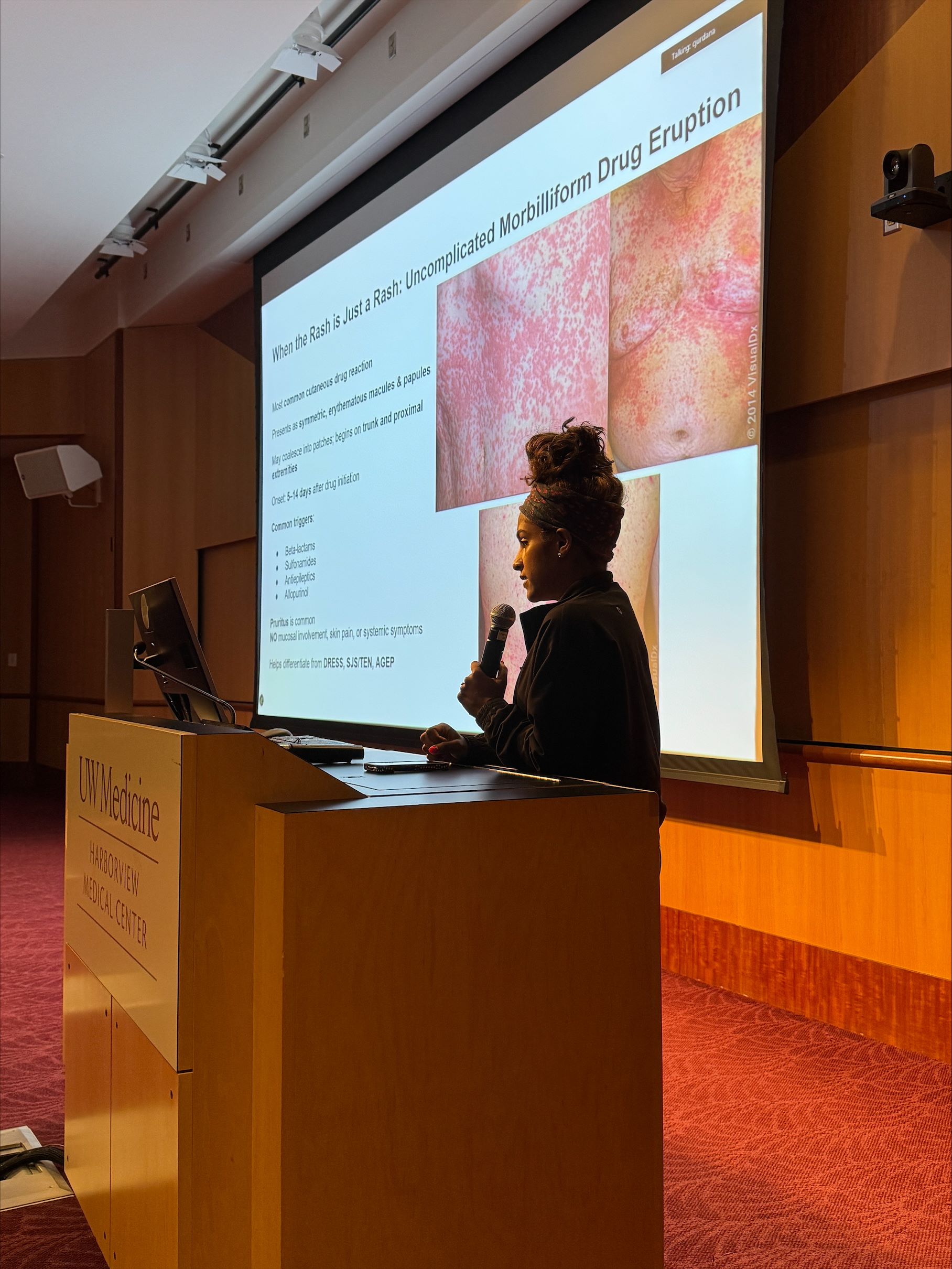
What did you teach the EM residents?
We focused on the dermatologic conditions that every emergency physician should be able to recognize and treat. This included true emergencies like Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN), Drug Induced Hypersensitivity Syndrome (DIHS), and Acute Generalized Exanthematous Pustulosis (AGEP), as well as more common but less severe drug eruptions.
We also covered how to appropriately prescribe topical steroids; we broke it down by potency, body site, vehicle, quantity, and duration. Lastly, we walked through common infectious rashes including viral, bacterial, and fungal, and discussed when to treat and when to reassure.
Why is it important for EM residents to learn about dermatology?
Emergency physicians are often the only line of defense. About 99.2% of hospitals in the U.S. don’t have inpatient dermatology services. That means emergency physicians are frequently the first and sometimes only providers making diagnostic and therapeutic decisions for skin conditions.
We wanted to ensure that wherever these residents end up practicing, they feel equipped to handle rashes with confidence, accuracy, and appropriate urgency.
How did you find the experience of teaching?
We absolutely loved it! It was energizing to step into a teaching role and share what we’ve learned over the past year. The EM residents were engaged, asked great questions, and had a practical mindset that led to some great discussions afterwards.
We especially enjoyed debunking common myths, like the fear over topical steroids or misidentifying morbilliform rashes as allergies. Their perspective pushed us to think about how dermatology fits into real-time, high-pressure decision making, and we walked away feeling inspired to keep building that interdisciplinary bridge.