Narrative Medicine Patient Panels Combat Bias & Burnout Through Storytelling


“Having HS affects you in the most profound ways, not just physically, but the toll it takes on your mental health and self-esteem,” said Brindley Brooks during a Hidradenitis Suppurativa (HS) Patient Panel hosted by UW Dermatology. “It really changes the way you feel about your body.”

Brindley, accompanied by her teenage daughter who also has HS, sat down with residents from the Division of Dermatology in early March to share their experiences living with and managing their chronic condition. At 44, Brindley described her long struggle to receive an accurate diagnosis, spending years keeping her HS a secret, and the shame and embarrassment associated with her condition.
“My whole experience with HS has made me so much stronger,” said Brindley, who is the Founder and Executive Director of HS Connect, a patient-led non-profit organization that provides support and resources to those with HS and the medical community. “Hopefully by sharing my story I can help educate the medical community and let people with HS know they aren’t alone in this.”

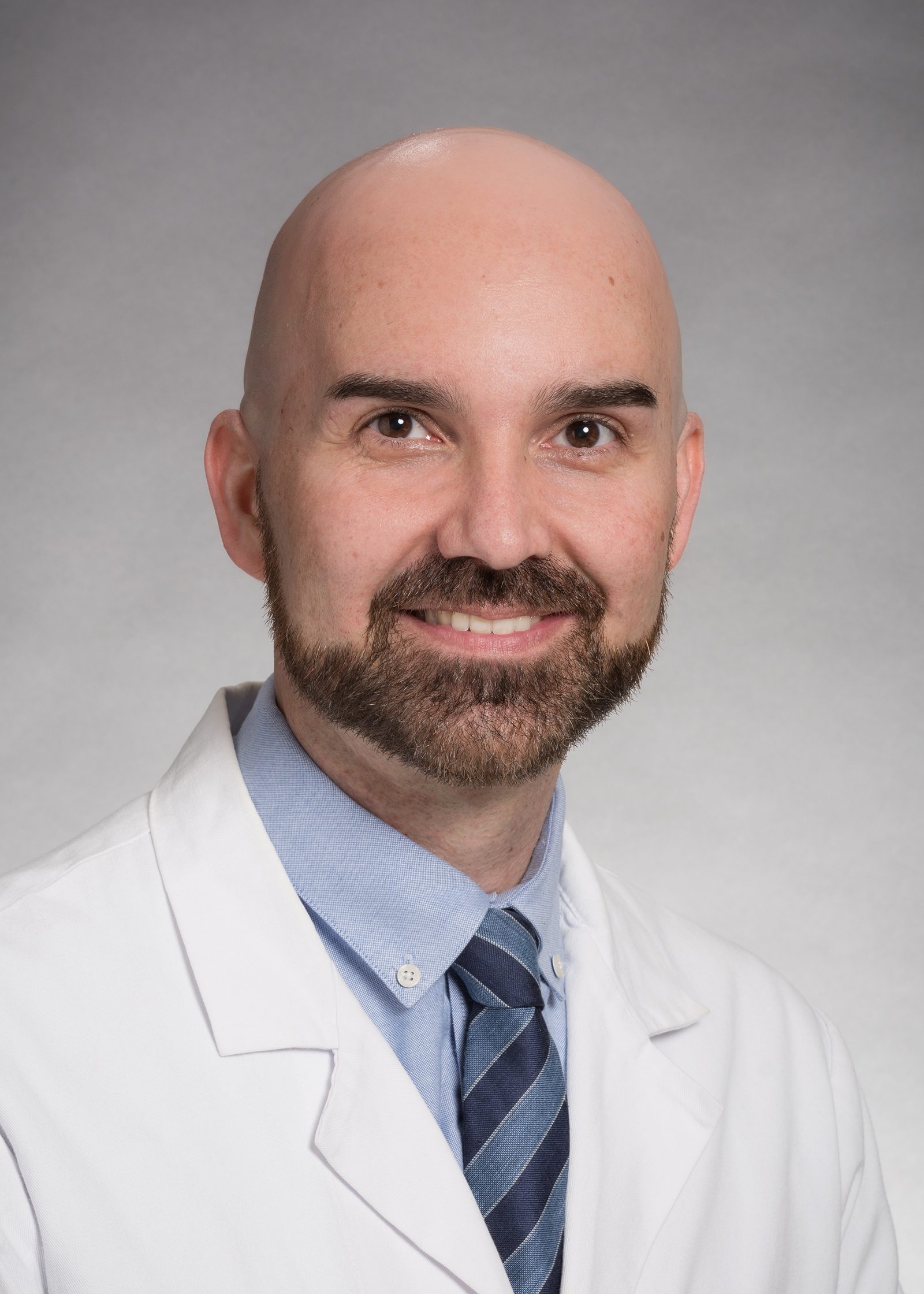
The HS Patient Panel was the second panel organized by Mariam Alam, MD, second-year resident and Caitlin Crimp, MD, third-year Co-Chief resident, for their collaborative research project, “Mitigating Bias and Burnout Through Patient-Centered Narrative Medicine.” In June 2022, Drs. Alam and Crimp received a grant through the Accreditation Council for Graduate Medical Education’s (ACGME) Back to Bedside program to develop a narrative medicine curriculum for dermatology residents, with the goal to improve residents' understanding and connection to patients and mitigate both bias and burnout.
Narrative Medicine is an emerging approach to health care that draws on the study of art and literature to enhance listening and observation skills. By exploring patient stories, context, and background related to illness, health care professionals can better understand each patient’s unique life experience, beliefs and values. Understanding a patient’s story can illustrate how they became ill, what caused them to look for care, and what challenges they face to get better. Rita Charon, MD, PhD, Executive Director of the Columbia University Division of Narrative Medicine, is widely recognized as the originator of the field.
Reducing Burnout Through Empathy & Self-Reflection

During each Narrative Medicine Patient Panel, residents are asked to read and critically analyze a piece of literature, poem or article related to the panel topic. Residents are encouraged to ask patients questions, and afterward are asked to write a brief self-reflection in response to a prompt, discussing what they learned and their thoughts, feelings and reactions to the panelists.
"The Patient Panels have been therapeutic for patients because it gives them the time and space to talk openly about their experiences,” says Dr. Crimp. “For residents, hearing these stories helps build empathy and a better understanding of what patients from different backgrounds go through.”
In the US healthcare system, doctor visits are generally short with little time for relationship-building with patients. Feeling less connected and the pressure to quickly diagnose before moving to the next patient has caused many health care professionals to experience burnout and lose meaning in their work.
Drs. Alam and Crimp recommend self-reflective writing as a tool to “cope with burnout and practice empathy,” especially if the patient interaction was challenging or stressful. There are no rules for self-reflective writing, just the physician's thoughts and feelings. These items would not be captured in a traditional chart note. For trainees, reflective writing also provides a “safe space” to freely discuss the stresses of medical school.
“We are better doctors when we have the space to be empathetic, and I think that can be lost when we are trying to see more patients,” says Dr. Crimp. “Hearing every patient’s story may not be feasible or necessary for every visit, but it could be just remembering to ask how the patient’s condition has impacted on their ability to do the social or physical activities they used to enjoy, or how it’s impacting their work. These questions you can incorporate over time."
"When I worked as a hospitalist, I cared for a husband and wife who had been married for 50 years and had both gotten COVID.” says Dr. Alam. “They ended up dying 24 hours apart to the minute. It was obviously a very stressful and emotional experience, but I found that sitting down to write about my interactions with them was incredibly helpful to process that.”
Addressing Racial Bias in Health Care

Another major focus of Drs. Alam and Crimp’s narrative medicine project is addressing the systemic racial bias and discrimination that continues to be found within health care. In Oct. 2022, Drs. Alam and Crimp hosted their first Patient Panel focused on skin of color. The patient panelist, a Black woman in her early 40s, shared her painful journey to diagnosis and how she began to research and advocate for herself.
“One of the themes from that discussion was that it took this patient a really long time to get to her diagnosis," says Dr. Alam. “Granted it was a very rare diagnosis, but she was dismissed repeatedly during the course of her care which led her to do her own research on her condition.”
The patient panelist described her frustration attempting to diagnose herself by looking for photos of her symptoms online. The majority of medical literature she found, however, was woefully lacking in photos of Black and brown skin.
“I came away from that panel thinking about how access to information can improve advocacy for patients and give them more autonomy in the decision making,” says Dr. Crimp. “She was great at self-advocating, but it was unfair in a lot of ways that the burden was placed on her. Patients who do not the same level of medical literacy that she did certainly fall through the cracks.”
The glaring lack of representation for skin of color can be found throughout dermatology journals, medical textbooks, research and clinical trials. For a specialty dependent on images for diagnosis, this has become a roadblock to proper treatment for patients of color and gaps in resident’s medical education.
“I think it’s important for dermatologists to understand the impact of bias in medicine because we deal with skin, the manifestation of race, unlike a kidney which you can’t see,” says Dr. Alam. “It’s particularly relevant because many of our patients have a visible condition that carry a lot of psychosocial burdens.”
One unexpected outcome of the Narrative Medicine project has been the increased connection among residents. Patient Panels give trainees the opportunity to meet in-person, get to know one another and discuss important issues facing dermatology. The program's success led Drs. Alam and Crimp to apply for a wellness grant through UW Medicine to fund an expansion of the Narrative Medicine program to faculty at UW Dermatology in the future.
“The feedback from our Patient Panels has been very positive, so our hope is that Narrative Medicine can become a sustainable part of our curriculum going forward,” says Dr. Crimp. "Ultimately we want to give residents tools they can use to self-reflect, check their biases and cope with burnout.”
Supplemental Reading & Viewing Materials
Gender Identity Panel — Lee Mokobe: A powerful poem about what it feels like to be transgender (YouTube)
Hidradenitis suppurativa (HS) Panel — The Pain Scale by Eula Biss
Skin of Color Panel — Excerpt from The Vanishing Half by Britt Bennett
HS Panel Patient Recommendations
Our HS Panelists shared several web and product recommendations for patients with HS.
Web Resources:
HS Connect — Created by people with HS with many educational resources including HS articles and blogs, video interviews and podcasts, product suggestions, mental health resources and support.
HS Foundation — Explore the HS Foundation website to learn more about HS. This website has excellent information about HS, its treatments, and links to support groups to connect with other patients with this condition.
Products: